Many Intended Parents turn to assisted reproductive technology after a cancer diagnosis.
Roia Barrios, Esq. Roia Barrios Surrogacy Law Firm

Many Intended Parents turn to assisted reproductive technology after a cancer diagnosis. Cancer treatment such as chemotherapy, radiation, and surgery can harm reproductive organs and affect fertility. For some women, being pregnant during or after a cancer diagnosis may be dangerous due to increased hormonal activity. And for some diagnoses, fertility preservation may not be possible at all. As a result, assisted reproductive technology plays an integral role in family planning after a cancer diagnosis.
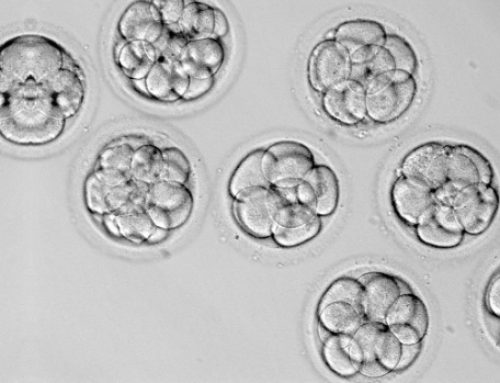
Oncofertility is a medical field that bridges oncology and reproductive endocrinology to maximize reproductive potential for cancer patients and survivors. As cancer treatments improve and survival rates increase, there is an increased focus on fertility preservation (and future quality of life). A cancer patient who intends to plan a family should consult with an REI, ideally before beginning treatment. A patient may have several fertility preservation options, including shielding, egg banking, sperm banking, testicular sperm aspiration, and embryo banking.
In cases where fertility preservation is not available, patients may use other avenues to continue their family planning, including egg, sperm, or embryo donations and/or gestational surrogates. A breast cancer diagnosis is one such scenario where it may be medically necessary that an Intended Mother use an egg donor and a gestational surrogate. Breast cancer is the most common cancer among women of reproductive age. Approximately 80% of diagnosed breast cancers are hormone receptor-positive: the cancer grows in response to estrogen or progesterone. Further, breast cancer treatment often causes premature menopause. During an egg retrieval, the hormone medication to stimulate egg maturation causes estrogen levels to rise and encourages the growth of hormone receptor-positive breast cancer cells. Because egg retrieval is potentially dangerous, an egg donor is often necessary.
In addition, women with hormone receptor-positive breast cancer are typically treated with five to ten years of endocrine therapy, such as Tamoxifen, following active treatment to prevent a recurrence. Edocrine therapy lowers estrogen levels or blocks estrogen receptors. The use of Tamoxifen is considered contraindicated during pregnancy because it can cause fetal abnormalities. Due to these complications, using a surrogate may be the best or only viable option for breast cancer patients.
While breast cancer may disrupt family planning, assisted reproductive technology may be a solution, and many Intended Parents have successfully navigated a cancer diagnosis.